THE COUNTER-SEXUAL REVOLUTION
The UK is facing a vast shift in the way we choose birth control. As the pill becomes less favoured for the first time in 50 years, what does the future of contraception look like?

More than three million women in the UK use the contraceptive pill as their primary form of birth control. When taken correctly it's over 99% effective at preventing pregnancies. There are 14 different options of contraception currently available, from the implant to the male condom to natural family planning.
In 2019, the NHS recorded that Britain’s most popular form of birth control had seen a decrease in its uptake. Its most significant drop in around five years. So something must be taking its place, and that seems to be increasingly taking the form of Long Acting Reversible Contraceptives (LARCs).
LARCs are defined by the National Institute for Health and Care Excellence as methods that requires fitting less than once per cycle or month. These include intrauterine devices (IUD), intrauterine system (IUS), injectable contraceptives and implants.
These four methods are a lot more physically invasive to the female body than simply 'popping a pill. However, there is still an attraction there for some women, such as the fact they last longer once inserted. Every woman, however, is different.
If this trend continues, what could the future of contraception look like? Are we shifting away from the burden of birth control lying exclusively on women, and are we about to witness the beginning of a counter-sexual revolution?
DAWN OF THE WONDER DRUG

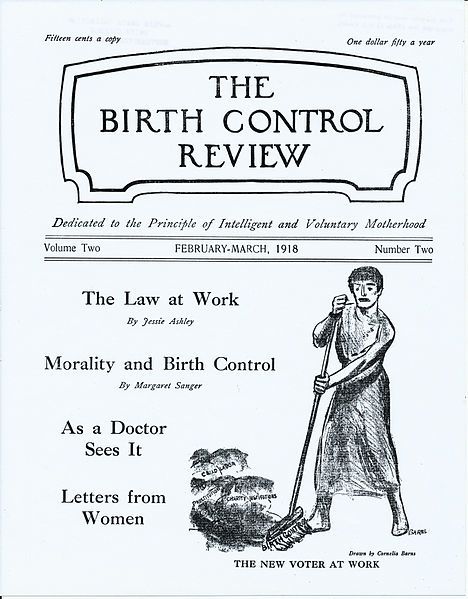
Birth Control Review from March 1918.
Birth Control Review from March 1918.
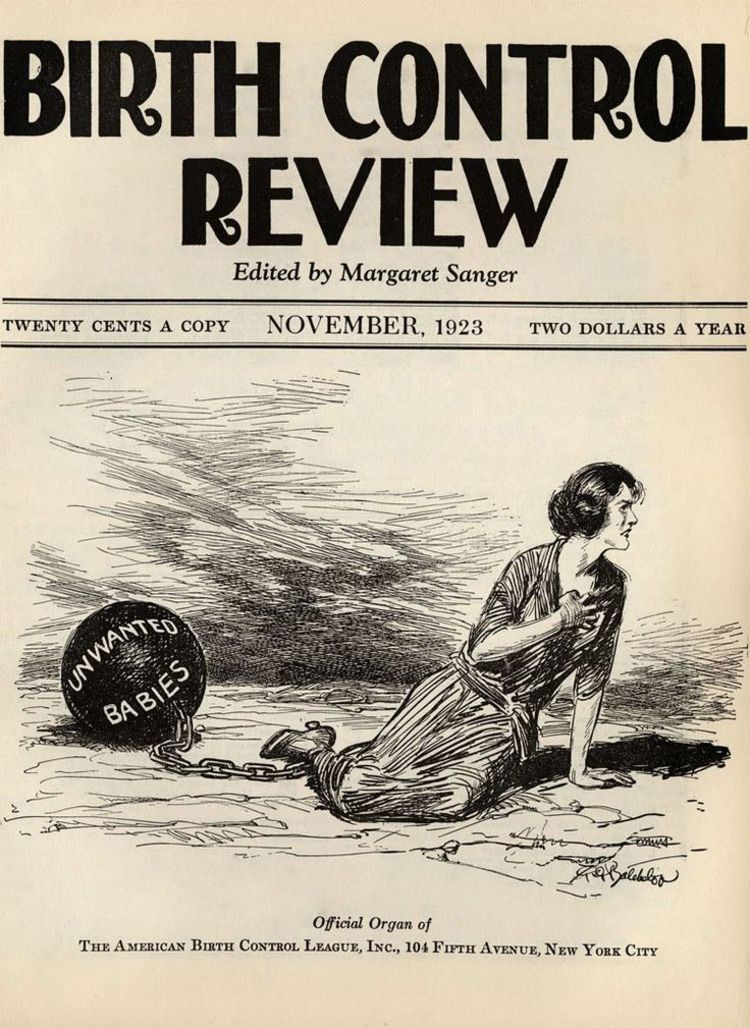
The Birth Control Review from 1923. One of Margaret Sanger's most famous editions. Picture credit: Peter K.Levy (Flickr.com)
The Birth Control Review from 1923. One of Margaret Sanger's most famous editions. Picture credit: Peter K.Levy (Flickr.com)

Portrait of Margaret Sanger.
Portrait of Margaret Sanger.
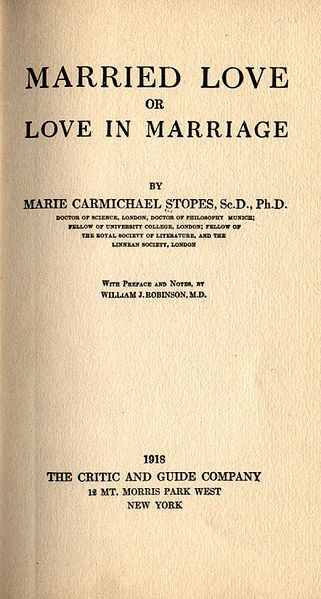
First edition of the book Married Love by Marie Stopes, 1918.
First edition of the book Married Love by Marie Stopes, 1918.
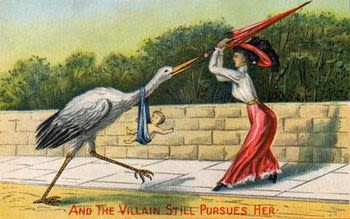
Satirical victorian postcard "The Villian Still Pursues Her". Picture credit: Uppity Rib (Flickr.com)
Satirical victorian postcard "The Villian Still Pursues Her". Picture credit: Uppity Rib (Flickr.com)
When the pill was introduced more than 50 years ago, it very quickly became known as ‘a wonder drug’. All of a sudden women took control over their choices and their bodies. A tremendous move away from the expectation to only marry young and raise children, when any kind of rebellion would be greeted with public humiliation and disdain.
Margaret Sanger was the first face to really make a difference on the birth control scene in the early 20th century. During her time of strenuous campaigning for women’s reproductive rights, Margaret started to publish the Birth Control Review, which had the ultimate aim of encouraging public support for the cause. The contents of the Birth Control Review promoted that women should have the right to choose motherhood, and have children according to the resources they could provide as a family, and the changing moral dilemmas surrounding these choices.
In the 1950s Margaret had met philanthropist Katherine McCormick, and together they funded and facilitated clinic research and trialling for the pill. On to this team came scientist Gregory Pincus and doctor John Rock, to begin to develop the drug. A drug which could stop women from ovulating.
It took Gregory and John until just 1957 to have successfully created the pill. At this point they were already aware of some of its potential side effects and worked tirelessly to try to reduce their severity.
With the help from Planned Parenthood Federation of America, the first birth control pills came into public circulation in 1961.
A pill that was made in just a decade and all without any government funding.
The 1960s brought in a sexual revolution. A social movement of many young men and women rebelling traditional norms surrounding sexual relationships. This sexual freedom, encouraged by the introduction of the birth control pill, has been illustrated in a poem called Annus Mirabilis by Philip Larkin.
It’s believed that during this trialling, Gregory stopped referring to the drug by its trademarked name of Enovid, but simply as just The Pill. Despite the many pills and tablets in circulation worldwide, he believed this was the only one that mattered. It's therefore hardly a surprise that a drug with so much importance is still to this day synonymous with contraception within our society.
A PRESCRIPTION CRISIS?

Statistics released by NHS Digital into the Sexual and Reproductive Health Services for 2018-19 revealed that even though the hormonal contraceptive pill is still the most popular form of contraception in the England, its uptake has slowed in the last five years. This decrease is certainly more of a steady one as supposed to a complete abandonment. Even though the drop may not be the biggest, it has been consistent year-on-year. Women are choosing to step away from the pill as their primary contraceptive.
The uptake of a contraceptive means that a new user has started using that form, albeit the pill or the contraceptive patch for example, as their main method of birth control. Uptake of the contraceptive pill was reported to be at 45% in 2014/15, but in 2018/19 was 39%.
At the same time, Long Acting Reversible Contraceptives have very slowly but also steadily been rising as a very real option for women as contraceptive methods. The four options of LARCs - which includes the IUD, the IUS, injectable contraceptives and implants - are types of contraceptives that only need replacing every few months. They are a commitment because of how much more invasive they act in the body, but where they may not be hormonal, their side effects may not be as detrimental as those of the hormonal pill.
In terms of the figures, it is worth noting that many young women will visit their local sexual health clinic about their LARC. This could be in terms of talking to a nurse about side effects or its pros and cons, or even to have it first applied or replaced. The statistics wouldn’t have picked up the items provided by sexual health clinics, and other reproductive health services - so it’s suspected this is not actually an accurate way of judging the full extent to which women in the England are currently using LARCs.
The graphs below will allow you to see for yourselves the extent to which young women are taking the main forms of contraceptives. You can click through the year groups and hover over the icons on all of the graphs to see how many young women are using each form.
The data below covers the last decade. The user-dependent element refers to the pill and contraceptive patch, and can even refer to the male condom.
THE PILL VS. MENTAL HEALTH

The makeup of the pill most commonly includes a mix of two main hormones: oestrogen and progesterone. These replace the natural hormones produced by the body with synthetic ones, but they essentially perform the same functions. There are two main types of contraceptive pill available to young women, of which they are prescribed according to any health conditions. The combined pill includes this mix of hormones, and is certainly the most common. Whereas some women will have to go on to the progestogen-only pill, or the mini-pill, if they have had anything from a history of blood clots to experiencing regular severe migraines.
The way in which these two pills act also differs.
The mini-pill simultaneously thickens the cervical mucus and weakens the lining of the uterus, which prevents the sperm from reaching the egg. As it only contains one of the hormones, the mini-pill contains the exact same dosage in each pill and so should be taken every day, with no breaks.
The combined pill however works to stop the ovaries from releasing an egg each month. To work at its best, the combined pill should be taken every day for 21 days, then you should take a week-long break to allow for a period-like bleed.
A Danish study published in 2016 looked into whether there could be a direct link between mental health issues and the taking of hormonal contraception. As it can be such a difficult thing to try to quantify, there is very little scientific proof that one can explicitly affect the other. Yet, such a large number of women report to have felt some kind of impact on their mental health which is more than the ‘mood changes’ or ‘depressed mood’ printed on the small-printed information leaflet inside the box.
The study used records of more than 1.8 million women between the ages of 15 and 34, and compared them across a 16-year period. This was made possible by the country’s unique PIN system, which tracks the history and medical choices made by each citizen.
The results found a 70% higher use of antidepressants in women that used hormonal contraceptives compared to those who didn’t.
They also found that across a year long period, eight out of 100 women would be users of antidepressants. But with hormonal contraception added into the mix, this rose to 14 out of 100.
It’s therefore more important than ever to recognise how the pill can have these detrimental effects on the day-to-day feeling of the lives of young women. Something that is supposedly an empowering drug shouldn’t come at such a cost.
"I was on the birth control pill for more of a decade of my life and I went off of it I felt very different. I felt more alive, I felt more vibrant, I had more energy, I started exercising again, I started becoming a different person and I really began to wonder whether the birth control pill might have had something to do with how I was feeling."
Dr. Sarah Hill is a professor of social psychology at the Texas Christian University, who has dedicated the last few years to the research for her book “How the Pill Changes Everything: Your Brain on Birth Control”.
Dr. Hill was on the pill for over 10 years and claims that she didn’t feel particularly bad during that time. She hadn’t experienced any worrying mood changes. However, it all changed when she made the decision to come off of it, and then to look into what exactly it had been doing to her over the last decade.

Dr. Sarah Hill
Dr. Sarah Hill
A lot of importance surrounding contraception and the pill for Dr. Hill is on the understanding of it. But it’s the increase in conversation that has really become the focus for her now.
"I have been really pleasantly surprised with just how ready women are to start having these conversations.
"I was concerned that at first in particular I was worried that people would misunderstand the message and think that I was somebody who hates the birth control pill and thinks that women shouldn't be on it, and that's not really my message at all.
"It's just about giving women all of the information that they need to be able to make informed choices.
"So I've been very, very pleased that most women seem to be, understanding the tone of the message and they understand like what the message is that I'm giving them and they're ready to start having the conversation."
In terms of the future of contraception, Dr. Hill therefore doesn’t think a complete abandonment of the pill is on the cards. But an increase in conversation and understanding of exactly what it can do to us. That’s the most important thing.
OUR CONTRACEPTIVE JOURNEYS

There is a significant lack of data providing statistical evidence for the impact of side effects of contraception on women. So it's difficult to put a figure on just how many women are suffering, or changing their form of contraception for these reasons, in England.
What we do know is that there has been decrease in prescriptions of the contraceptive pill, and an uptake in LARCs.
But with more and more women turning to social media and creating support groups to share their contraceptive experiences, the real-life impact of these side effects has to contribute to explaining these figures.
Below are the stories of six women, who have used a variety of forms of contraception. As birth control is often something a women will experience for around a decade of her life, it isn't just an experience but a journey.
Click here to go to the stories of these women!
Click here to go to the stories of these women!
Click the image above to go and read their stories, as well as how a GP judges what the best course of prescription is according to their patients.
SHAKING UP SEX-ED
The biggest influence on how women choose their contraception and what they know about its varying forms comes from their sex education experience in schools.
Which contraceptive option many women start with often stems from what they remember from school, or they may even make these decisions whilst still in school.
Schools in England have a legal duty to teach some form of sex education to all pupils, which will also include topics including relationships, consent and contraception.
Zoe Fish works for the School Public Health Service in Sex and Relationship Education, as part of the Kent Community Health NHS Foundation Trust.
Her job includes training staff to make sure sex and relationships education is provided in every school in the county to the best quality, and planning so that teachers can deal with every scenario in potentially sensitive areas of their teaching.
A school’s curriculum is, however, always changing and developing.
In 2014, Parliament turned down a vote to make sex education, including topics such as relationships and consent, a compulsory element of the curriculum. However, the topic of changing the sex education curriculum didn't disappear from the government's agenda. Three years later in March 2017, the Education Secretary of the time Justine Greening, announced a legislative change to how sex and relationships education would be taught in schools.
Section 34 of the Children and Social Work Act 2017 states how these changes will be taught in all schools across England. This change will mean that this area will now be regarded as 'Relationships and Sex Education' (RSE), and will teach relevant content from a younger age, and will set the quality of teaching for all schools in England to facilitate.
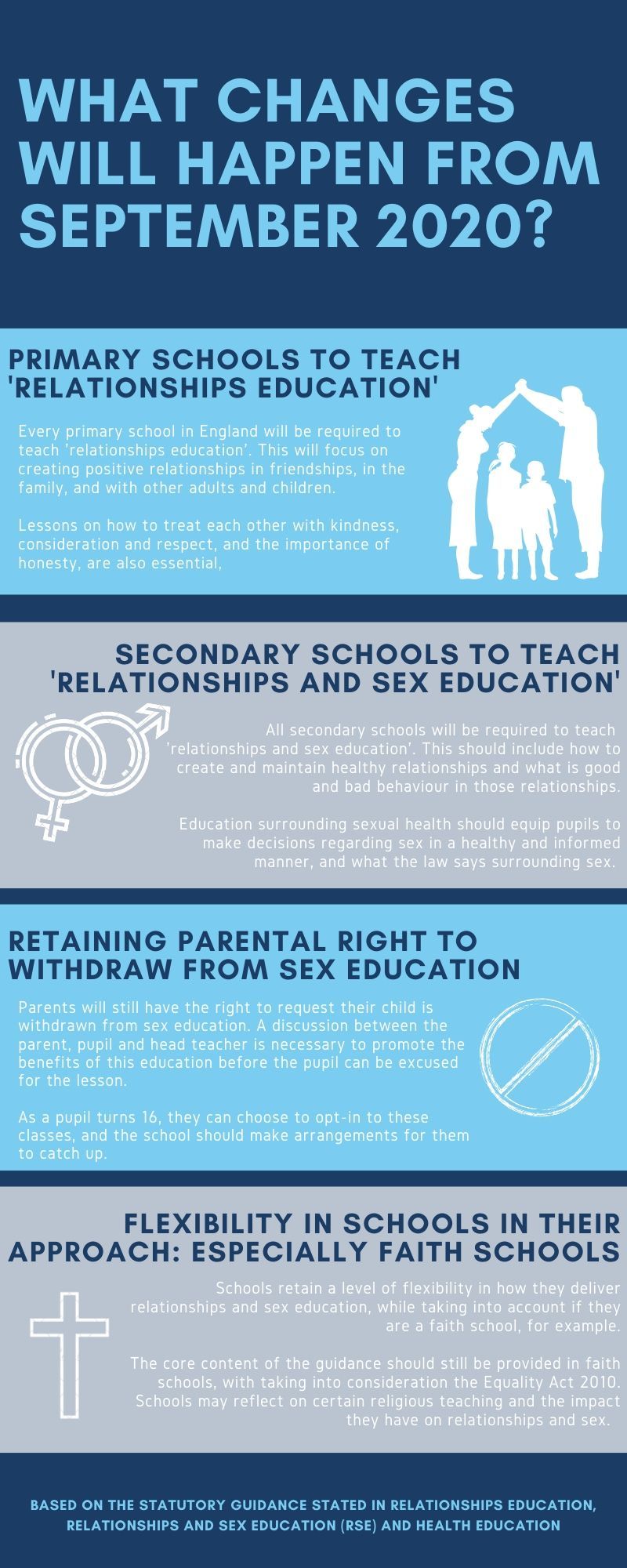
The statutory guidance for teaching relationships and sex education has developed to fit these changes, so that it is no longer just a choice by some school leaders to contain this education in their PSHE education.
These changes are to be implemented in the next academic year starting from September 2020. Zoe Fish talks about how this new Relationships and Sex Education legislation translates into a real classroom.
We won't know how effective the changing curriculum will be for a while, but hopefully a better quality of relationships and sex education will make young people more aware of how they should conduct themselves and the responsibilities that sex brings.
In terms of contraception, mistakes will still happen. Regardless of how well the contraceptive options are taught and provided to young people, it is almost inevitable that slip ups and mistakes are made. It's part of the learning curve.
So what happens to a woman when a mistake is made, and she needs to quickly prevent pregnancy?
THE PLAN B

One thing that was mentioned by Zoe Fish was an uncertainty surrounding how much emphasis is put on emergency contraception in schools. The morning after pill is an essential element of contraceptive options in the UK, in providing means of preventing unwanted pregnancies.
But just how available is emergency contraception?
The #JustSayNon campaign was initiated by the British Pregnancy Advisory Service in response to numbers of women complaining that barriers to accessing the morning after pill had resulted in unplanned pregnancies.
'#JustSayNon campaign video - British Pregnancy Advisory Service'
Katherine O’Brien is BPAS’ Associate Director of Communications and Campaigns, and she believes the price point of the pill is ‘prohibitive’ and needs to be lowered so the women who need it can get it.
The campaign faced a lot of backlash from the health and beauty retailer Boots, but their backing down and promising of a cheaper generic to their morning after pill was one of the greatest achievements of this campaign.
After issuing bpas two legal warnings over our campaign, we welcome with Boots' announcement. Comment: https://t.co/BpR5ES910S #JustSayNon pic.twitter.com/A68nJZwd2O
— bpas (@bpas1968) August 31, 2017
Following the success of the campaign, the next step for BPAS is to tackle the stigma surrounding the consultation element which has to happen with the pharmacist before the morning after pill can be given.
While the consultation may help some women in seeking advice about their method of contraception and how to avoid using emergency contraception repeatedly, it’s widely believed that this is just an awkward step that women should have the choice to opt in or out of.
In December 2019, a YouGov survey asked if the rules could be changed to remove this consultation, would people want to see that change?
"It's hard to imagine anybody talking about men accessing Viagra and things like that, which you can now do online or in-store, just to pick them up with no hassle or consultation. Boots very proudly advertise this service. It really shows just how women’s sexuality is still being policed."
BPAS are in conversation with drug manufacturers to work towards challenging the licensing that only pharmacists can access emergency contraception. Just how long these changes will take to come about are still uncertain.
"It's quite patronising and demeaning. It's hard to imagine any kind of male medication being policed in that kind of way."
Katherine O'Brien says: "It's this idea that our sexuality needs to be policed, it needs to be regulated. That ultimately there is somebody else that has this information that we don’t have, and that we’re all just walking around aimlessly waiting for a pharmacist to tell us about the pill.
"It's quite patronising and demeaning. It's hard to imagine any kind of male medication being policed in that kind of way."
Besides the access issue, a lot of women have said they sometimes don't feel comfortable even using the morning after pill when they need it because they don't trust how safe it is on their bodies.
“I think that there is a lot of confusion about the morning after pill in terms of its safety, because it is a very safe method of contraception. Even if you took it and you were already pregnant, it wouldn't do anything to harm your pregnancy."
ellaOne is the most used brand of emergency contraception currently in the UK. They’ve decided to tackle misinformation of the morning after pill head on, and recently released their Fact Not Fiction campaign. Below is one of their four main TV adverts.
'Fact Not Fiction Campaign TV Advert - ellaOne'
As we have now been ordered to stay at home by the government in the attempt to stop the further spread of Covid-19, just how long we will have to stay indoors is unknown. This will make getting hold of repeat prescriptions for contraceptive options more difficult. Therefore BPAS is encouraging all women to order the morning after pill to use at their disposal from home in the meantime to prevent unwanted pregnancies.
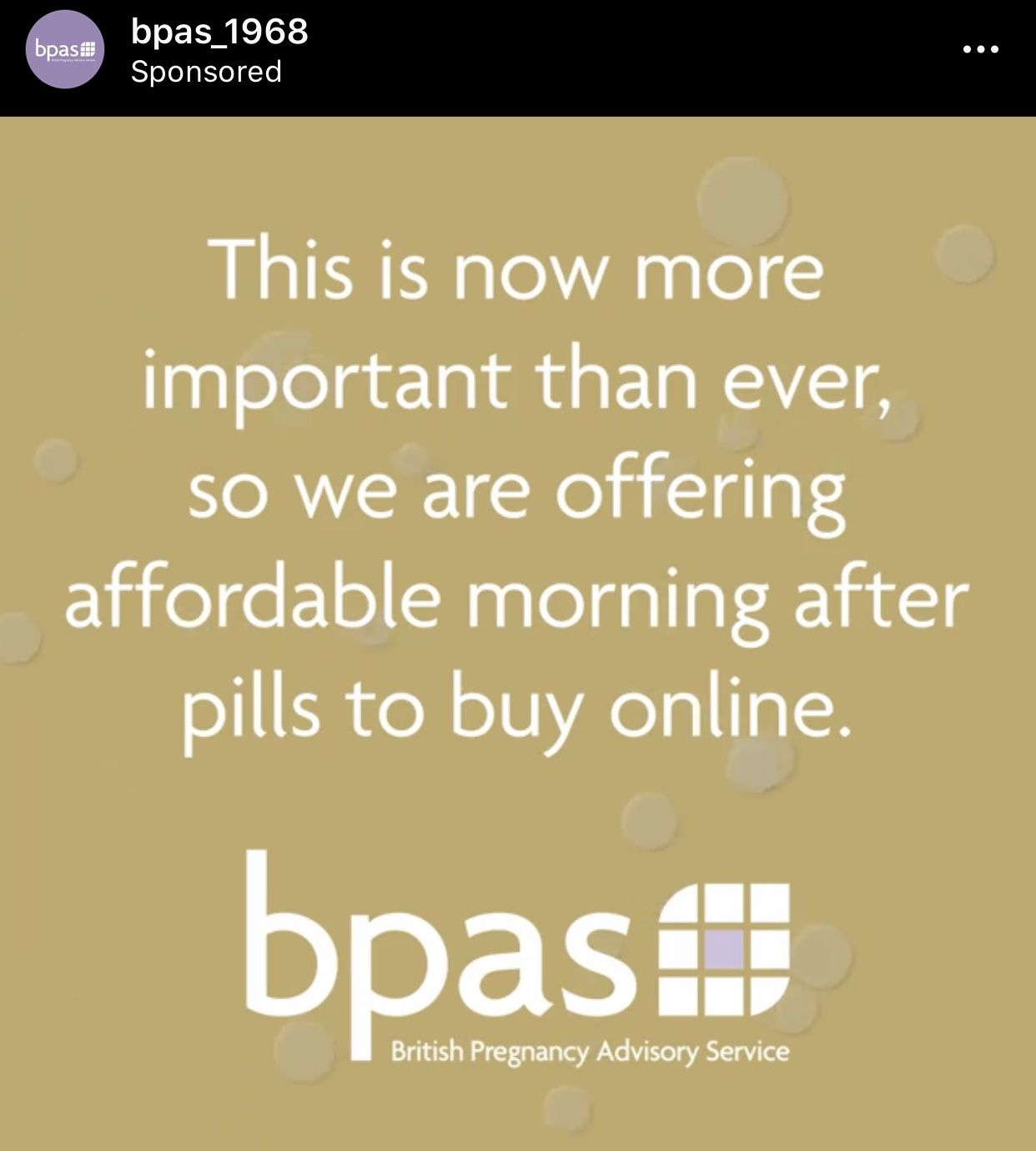
Sponsored instagram post from @bpas_1968
Sponsored instagram post from @bpas_1968
SHARING THE BURDEN
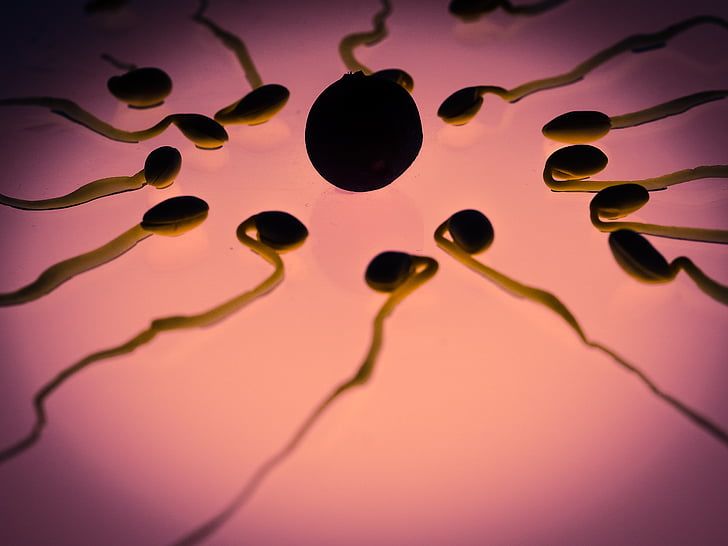
All of these options very much put the duty of birth control on the female, even though everything up to this point includes both a male and female. Is there a way that this responsibility can be shifted in the future, to ease the pressure away from women?
One in three men say they'd consider using a male alternative to the female contraceptive pill if it became available, according to a YouGov survey.
The University of Edinburgh is currently the leading recruiting centre worldwide for couples to clinically trial a male contraceptive gel. The trials are being organised in the United States and are funded for by their National Institute for Health.
Research in to some form of male contraceptive have been going on since the 1970s, taking the forms of a pill, injection, and now a gel.
Richard Anderson is leading these trials at the University of Edinburgh. Click through the questions below to find out more about how the gel works, and how the trials are being run.
However, these things take time.
Even though when the pill was first trialled in the 1950s it only took a decade before it become widely available, in the present day these trials are expected to take much longer before they can come into fruition due to funding.
Professor Anderson recognises this has been a 'slow process'.
"It's been a long process hasn't it. And it is frustrating, you say well if it worked 20 years ago how come there's still not a product on the market. But I think those were like prototype versions, you go to a manufacturing facility and they generate a prototype that's never going to be for sale but it demonstrates it can work and it's been a bit like that.
"But it's been a slow process turning it in to something that could work. But this daily gel could, if it works really well, could then be something that is then out there and available for people."
If the male contraceptive gel is proven to work, a commercial partner will still need to be found to market it. Professor Anderson believes there is a need for a new male contraceptive, especially in long-term, trusting relationships.
With the changing situation presented by Covid-19, the decision has been made that these trials will continue. None of the centres worldwide are allowed to recruit anymore couples as a result, but at 50 or so couples, Edinburgh is still the leading recruiter.
THE FUTURE OF CONTRACEPTION IS...

This new male contraceptive may still take years to become available, and that is assuming all goes well with clinical trials. The burden of preventing pregnancy still majorly lies with the woman.
Seven in ten women (70%) think women tend to take more responsibility, but just 40% of men agree, according to a YouGov survey.
Arianne Shahvisi is a Senior Lecturer in Ethics at the University of Brighton, who is currently conducting research into the sex inequality of contraception within relationships.
"So I’ve been examining that inequality and looking statistically at what the future might look like in terms of perhaps moving towards male long acting reversible contraception and what men’s attitudes should be towards those from a moral perspective - them kind of stepping up taking responsibility so that women don’t have to take responsibility for contraception, as well as worrying about the burden of pregnancy."
Arianne Shahvisi
Arianne Shahvisi
If a male contraceptive gel does become available in the foreseeable future, there will be a shift in the conversations happening between men and women about how they will manage birth control.
If a woman is unhappy about her contraceptive, hopefully at some point in the future, that burden may be on the man.
Women shouldn't be the sole-bearers of the responsibility when there are two individuals involved.
We've seen a number of women complaining about the form of birth control they are put on, and either putting up with or having the strength to change it. Sometimes more than once. In the hope that maybe there is an option that they can feel happy, settled and ultimately safe with. But the statistics show that not a lot of women actively 'shop around' for contraceptives.
Helen Clayton GP said that she doesn't notice many of the women who she prescribes contraception coming back consult on their options.
"It is fairly unusual for them to come and say ‘actually I’d like to try something else’. I can’t think of a percentage but its relatively unusual. If they’ve tried it and they don’t like I’m very happy to switch them to something else, because obviously it's important that they’re protected against pregnancy, if they’re not taking the pill happily, they’re not going to be protected."
Arianne believes this can be due to a lack of education about what options are available and how they could react to them.
If the current burden of preventing pregnancy is causing this level of issues for women, can there ever be a shift towards men taking up this greater responsibility? Arianne believes this will have to come from sex education in schools, to make sure men are aware of the part they play from a much earlier age.
"I think actually it's also going to come down quite a lot to how sex education is carried out in schools, so I think with the introduction of these new male long acting reversible contraceptives, what we might see it a very, very different emphasis in terms of what is expected of young men.
"So we might see a new generation of men growing up where it's the norm that they would ensure that they cannot make somebody pregnant, or that they minimise the risk of that occurring, and then a new generation of women may then have a very different perspective on having sex with those men.
"I think we’ve got to look at the fact that this may shape social norms so while at the moment some women might struggle to see how they would trust a man in this scenario, that doesn’t necessarily say anything about how the next 10, 20 years will look in terms of how people have sex and take responsibility for it."
Taking everything into consideration, one thing is certain - change, if it isn't already happening, needs to.
The male condom is still the most efficient method of contraception to protect both parties from sexually transmitted infections. When it comes to pregnancy, it isn't fail safe.
Women are becoming increasingly frustrated with how contraception affects their mental and physical wellbeing, and even if they do find an option that they get on well with, it can take a lot of experimenting which can take its toll. What can all of this mean for the future of contraception, looking forward?
The trends certainly seem to suggest that women are either not turning to the pill straightaway as their primary form of contraceptive, or that they're brave enough to know when their body has had enough and they need to try something else.
Whichever the explanation, this pattern is a continuing one, and it doesn't show any signs of reversing. If so, the contraceptive pill is becoming less of a 'wonder-drug' and more of a dread for many women.
Long Acting Reversible Contraceptives could be replacing the pill as the most popular form of birth control within our lifetimes, and the burden of preventing pregnancy may become more of a shared experience within a relationship.
What this means for more casual encounters is uncertain, as condoms will always be the most effective way in preventing sexually transmitted infections.
But one thing is for certain. In England, the scope of birth control is slowly changing. We are witnessing a change in behaviour, and this has to be translated in schools and in wider society. Women will not tolerate or put up with the burden or responsibilites placed on them because of their sex any longer.
This is a time of change, and a counter-sexual revolution.
CONTRIBUTORS

Jennifer Forrest
This project would not have been possible without the amazing perspectives all these people have provided. Their honesty has been admirable throughout, and without it we wouldn't have been able to work together to tell the story and fully investigate the issues that contraception is creating in the UK, which is key for looking forward to work out what the future of contraception could look like. Thank you!
Produced and written by Jennifer Forrest.

Dr. Sarah Hill
With thanks to:
Dr. Sarah Hill

Helen Clayton GP
Helen Clayton GP
Lizzie Trott

Lizzie Trott
Rhiannon Carter
Jenni Cartwright

Rhiannon Carter
Roxanne Bevan
Kiele-Ann Dunne

Jenni Cartwright
Mollie Manning
Zoe Fish

Roxanne Bevan
Katherine O'Brien
Professor Richard Anderson

Kiele-Ann Dunne
Arianne Shahvisi
Additional photo credits:

Mollie Manning
Bethany Wong
Reproductive Health Supplies Coalition on Unsplash

Professor Richard Anderson
Benjamin Moss on Unsplash
Poem: Annus Mirabilis by Philip Larkin
NHS Digital statistics based on findings found here.
Arianne Shahvisi
University of Copenhagen study linking contraception and depression can be found here.
YouGov survey about the morning after pill can be found here.
YouGov survey about male contraception can be found here.

Jennifer Forrest
Jennifer Forrest

Dr. Sarah Hill
Dr. Sarah Hill

Helen Clayton GP
Helen Clayton GP

Lizzie Trott
Lizzie Trott

Rhiannon Carter
Rhiannon Carter

Jenni Cartwright
Jenni Cartwright

Roxanne Bevan
Roxanne Bevan

Kiele-Ann Dunne
Kiele-Ann Dunne

Mollie Manning
Mollie Manning

Professor Richard Anderson
Professor Richard Anderson
Arianne Shahvisi
Arianne Shahvisi


