COUNTER SEXUAL REVOLUTION:
OUR CONTRACEPTION JOURNEY

In order to be prescribed the pill, or any form of contraception, a young women will need to have a consultation with her GP first. These forms of contraception cannot just be purchased over the counter like the male condom.
In this consultation, GPs are advised to discuss with the woman her options and what she thinks is best for her, so that the decision is a joint one.
Helen Clayton, GP at The Oaks Surgery in Swanley experiences prescribing the pill to first-time users on an almost weekly basis.

Helen Clayton GP
Helen Clayton GP
She doesn't believe in just handing over the pill to women, and that a conversation has to happen to make sure women feel like there is always an open door for them.
If a woman is uncomfortable with her prescribed form of contraception, or is having a prolonged bad experience, she has every right and desire to change that form. Especially when there are so many options available. But what happens when the initial advice and prescription by the GP is no longer good enough?
Below are the stories of six young women who have had varying experiences with varying forms of contraception.
RHIANNON CARTER: THE PILL
21, STUDENT
Lots of young women can find themselves taking the pill before they need to start thinking about contraceptive options, for a variety of different health reasons. At the age of 17, Rhiannon Carter was one of them.
Rhiannon’s first introduction to the contraceptive pill came in the form of Rigevidon, one of the most popular ‘brands’ of the combined pill. She felt as though she didn’t suffer from any side effects and felt safe taking it.
“The stories other people had about its side effects did freak me out a little, but I did trust the doctors and because the check ups were more regular I knew that they would look for any side effects just in case.
“So I felt pretty comfortable taking it.”
When Rhiannon started life at university, her doctors started by deferring from the pill she has always been prescribed.
They switched my contraceptive pill four times in the first two years of my degree."
There are numerous types of pills which come under the family of the combined pill. In theory they all behave in the same way in that they include both the oestrogen and progestogen.
However it isn’t just the brand names which change, so can the ingredients they contain.
To start with, the change went from Rigevidon to Levest - a brand of pill many consider to be ‘cheaper to the NHS’.
As Rhiannon had only ever tried Rigevidon and had good experiences with it, the change this took on her mentally was a shock to the system. She managed to stick it out for a year until her next pill review with the doctor, where she first mentioned all of her symptoms.
"They switched my contraceptive pill four times in the first two years of my degree.
“I was having horrendous mental health issues, bloating, breaking out etc., and yet when I went to the doctors, they would not listen and instead would blame the ‘student lifestyle’ for my symptoms.”
After her complaints about Levest, the review resulted in yet another change. This time to Marvelon which ‘was definitely the worse out of all of them’.
“My symptoms included severe headaches and migraines. Stomach cramps. Severe mood swings and poor mental health to the point that there would be weeks where I wouldn’t leave the house. Just about every side effect they list as being ‘mild’ on the information leaflets I experienced. And they were not mild.”
Despite this huge affect the pill was having on Rhiannon’s day-to-day life, she didn’t go to the doctors to change it.
"They didn't listen to what I had to say. They 'knew best'."
Considering this was now her third pill change in the space of two years, she felt they’d stopped listening to her.
“I felt as if I was annoying the GP surgery by constantly complaining so was reluctant to do or say anything about it even though I was genuinely struggling.
“It came to a point where I found it difficult to socialise or do anything active which just wasn’t OK.
"They didn't listen to what I had to say. They 'knew best'."
Rhiannon finally spoke to a nurse at a sexual health clinic who sympathised with her experiences. Her next prescription was for Gedarel, which was somewhat an improvement but things didn’t return to normal. It was the optimism from this discussion which made Rhiannon feel like something good was finally going to get done. She made an appointment to discuss all of her side effects. She was finally getting listened to and taken seriously.
“He listened to what I had to say and comforted me. He then recommended I be put on Rigevidon as my body never had an adverse reaction to it. He also put a note on my medical record that I only be prescribed Rigevidon in the future.”
This constant changing between drugs really began to take its toll on both her body and her mind.
“I never had any serious side effects from the pill I was on, which was Rigevidon, but on the three others I was put on, I experienced every side effect under the sun.
“Being a woman is hard enough when people think you overreact to most things, but being told you are overreacting about symptoms you’re having was the final straw.”
Rhiannon had to try four variations of the contraceptive pill.
Rhiannon had to try four variations of the contraceptive pill.

"They would blame to 'student lifestyle' for my symptoms."
"They would blame to 'student lifestyle' for my symptoms."

Lizzie was changed to the mini-pill after experiencing migraines.
Lizzie was changed to the mini-pill after experiencing migraines.

"I'm a slave to the pill."
"I'm a slave to the pill."
LIZZIE TROTT: THE PILL
26, Accounts Administrator
Regardless of how many contraceptive options are available to women, there is still a shared feeling that it's something we, as a gender, have to just put up with. For some, there is no reassurance that there is an option perfect for them. For Lizzie Trott, there is a sense that she will always be stuck with the pill, and that there is no miraculous alternative for her.
Lizzie started on the combined pill aged 16, in an attempt to solve her issues with heavy and painful periods. This worked, as she almost instantly saw her periods become much lighter.
"At first it was great, I had no problems. I loved the freedom of knowing when my period was due and being able to postpone it by taking pills without the seven day break.
"My skin was clear and I felt in control."
Taking the pill also fitted in with Lizzie's lifestyle. At the time, Lizzie was training to be a professional dancer, so the element of control at this point, was essential.
“Being able to go ‘oh well I’ve got this tour coming up so I’ll just put all of my pills together and I won’t take the break’, was ideal.”
Lizzie was using the combined pill as her primary form of contraception for seven years, but it was only in the last two she started feeling the side effects, which eventually pushed her and her doctor to make a switch.
“I never really had any symptoms and I took it probably until I was 23, and then I started slowly getting migraines and it took me ages to figure out that it was on that seven day break so it must have been that drop in oestrogen, which was causing these almost withdrawal headaches.”
Her doctors started prescribing her onto the mini-pill as a result of the migraines, which Lizzie was not impressed by.
“I was changed to the mini-pill, which I did not relish the thought of as my mum got pregnant with me on this pill.”
This was the first time in about six years there had been a change in Lizzie's contraceptive journey.
“I wasn’t thrilled about it.”
"I was changed to the mini-pill, which I did not relish the thought of as my mum got pregnant with me on this pill."
Another concern which made Lizzie anxious about the mini-pill was the horror stories she’d heard from friends.
With some women, the mini-pill can cause breakthrough bleeding every couple of months, due to the thickened lining of the womb. This bleeding was something Lizzie felt she needed to avoid at all costs.
"I was most worried about breakthrough bleeding because I work in such a male-dominated industry, so I work for a haulage firm, and at the time I started there, there was only four women in the whole business out of 60 employees.
“To get to our toilet you have to walk through the workshop where they stick some lorries, so the idea of having a bleed that may have soaked through your trousers then having to walk through that to get to the toilet to sort yourself out, was honestly the worst thing ever.
“I was terrified that that would happen!"
The same issue of breakthrough bleeding can happen with many of the LARC options too. Lizzie spent time researching these, but she decided they were too invasive only to have the same result.
“I gave it a go. It has been a very hard two or so years adjusting to it.
“I’m glad my periods have gone because I never wanted that, I had never got on well with it."
In terms of side effects, Lizzie suffered badly.
“I got, and still have, hormonal acne which was a learning curve, and all my hair started falling out.”
It took a few years for Lizzie to experience any side effects on the combined pill. For the mini-pill, Lizzie deteriorated quickly, and a lot worse than before.
"I got, and still have, hormonal acne which was a learning curve, and all my hair started falling out."
“Because there's no kind of peak or trough with the hormones, you don't really get a break from it. It's just constant.”
Below you can see photos from before and after Lizzie's taking of the progestogen-only pill, to see just how it’s affected her skin.

Two years on, and Lizzie is still unhappily taking the mini-pill.
“But I know in my heart I’m a slave to the pill.”
She finds it entrapping but feels like she doesn’t have much of an option to either stick it out or completely abandon it.
“Currently I am considering coming off of it altogether, and just using condoms.
"I’m sick of the acne and I’m hoping perhaps my body will now be able to figure it all out on its own.
"But I know in my heart I’m a slave to the pill.”
A lot of women react incredibly differently to the pill, in each of its forms. In the box they come in, the information leaflet contained gives a gist as to what side effects women should expect to feel.
Helen Clayton GP says that she encourages girls to be aware of all of the potential side effects before even beginning their first course of the pill.
"The side effects in the box, and I do always encourage girls to go and sit down with a drink and read whats in the box, because I think its important that it reinforces the discussion that we’ve had.
"I mean I think it helps if before you start anyone on something that you explain the side effects to them, because if you’re expecting your boobs to grow and feel uncomfortable and feel a bit sick for your first couple of months of taking the pill, you’re much more likely to tolerate it than if no-one tells you that.
"So explaining the side effects and how long they’re likely to last, and that they’re normal and they usually wear-off, that can often get people through those early days."
Below are those side effects leaflets, taken from one brand of combined pill, and a brand of mini-pill. It should also be noted there are variations between brands of pill due to ingredient changes, regardless of how minor they are.
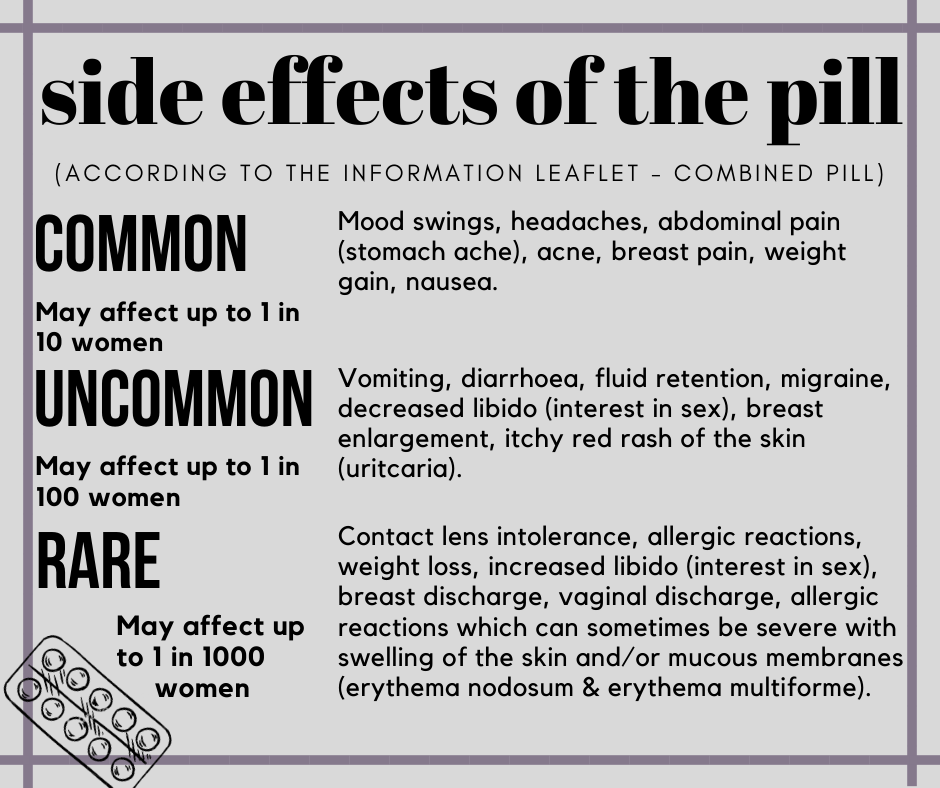
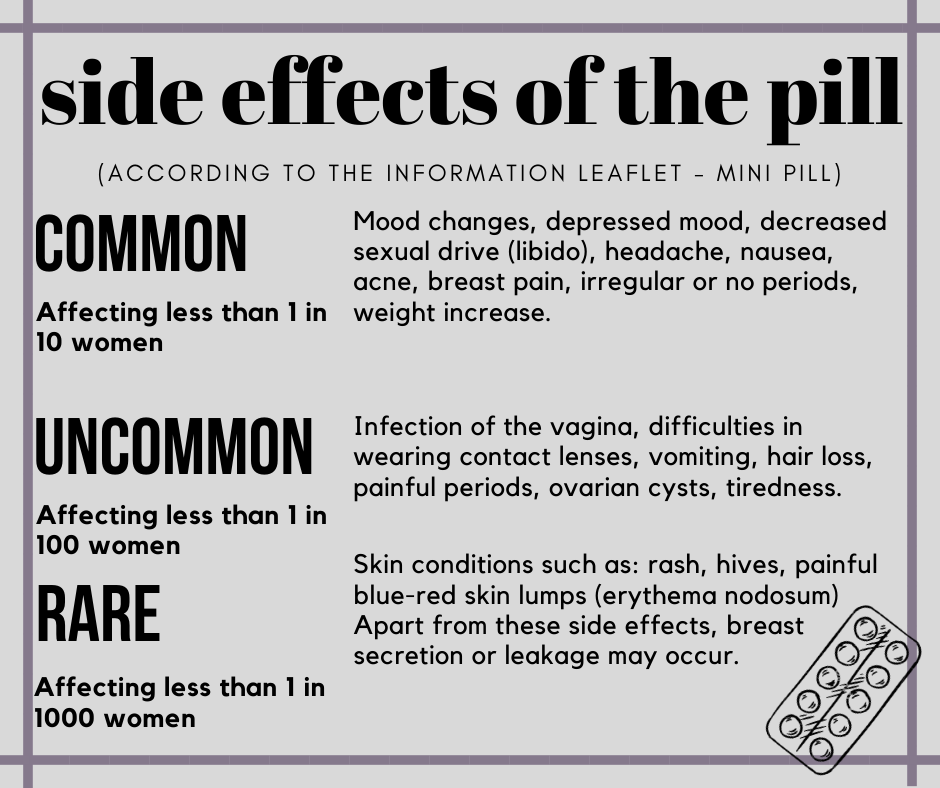
On both of these leaflets, the mental health issues that so many women reported are labelled as 'mood swings', 'mood changes' or 'depressed mood'. Are pill manufacturing companies failing to supply women with knowledge of just how significantly these pills can affect a woman's mental health, or are they just in denial about the real-life experiences these women are having?
JENNI CARTWRIGHT: THE IMPLANT
22, STUDENT
When Jenni first took birth control into her own hands, she did her research into options available to her before settling for the Nexplanon implant.
“I didn’t want to have to worry about contraception so the thought of taking something every day for a certain period of time was a no from me, because I’m forgetful and if you forget to take the pill then it’s obviously a bad thing.
“So I looked into it and I went for the Nexplanon implant, just gets popped in and I don’t have to worry about it.”
Once the implant is fitted it lasts for three years. Within its first year, Jenni’s side effects were really starting to have an effect. But as her first ever form of contraception, it took a while for her to realise that the symptoms she was experiencing could be linked to the implant.
“I had some issues with it though like mood swings, weight gain, depression, lack of sex drive and anxiety but I didn’t realise it was the implant doing that to me until about a year in, and by that point I was so used to it that it felt like that was just me now, so I finished the three years on it.”
Just before those three years were up, Jenni naturally turned to contacting her GP surgery to make an appointment to discuss her side-effects and what should come next. But there was an issue. A reoccurring issue. Having begun to process of making an appointment in September, she wasn’t offered one until the following February.
Jenni had her implant removed by the local sexual health clinic straight away, as it had reached its expiry and didn’t have time to wait for a doctors appointment.
"When I need it replaced again I’ll go straight there.”
Despite the stress of not really knowing where to go, Jenni had a far better experience at the sexual health clinic than she'd ever had at the doctors.
“They were also so friendly there the two nurses chatted to me the whole time and were very professional with extracting and replacing, took about an hour from arrival. When I need it replaced again I’ll go straight there.”
However, she was still needing to speak to someone about her next prescription.
"I wasn’t prepared to mix hormones and experience new or different symptoms.”
Having waited for months to get an appointment, the day finally came. She had done three months without a contraceptive besides condoms, despite the clinic offering her the pill in the meantime.
“For the interim period between the implants they offered me the pill but I didn’t take it, I just used condoms. I wasn't prepared to mix hormones and experience new or different symptoms."
Jenni was faced with a decision as to whether or not she was going to stick out the implant for another three year period, or try out a new form of contraceptive. The implant’s main attraction was that once it was in she could forget about it in terms of birth control, and that it eased her once painful periods.
“But the weight gain and mood swings were a big upset for me.
"I’ve been with my boyfriend for five years so I got the implant a year into the relationship so we didn’t have to worry about contraception and he was fully supportive but when it became the time to have it taken out he suggested something different as he saw how if affected me.”
As much as medical professionals aren’t responsible for the decisions young women make about their contraception choices, they certainly can play a significant role in how they make the decision.
When her appointment came around, she felt like she wasn’t given much in the way of information about alternative forms of contraception which could have made her choose to step away from the implant altogether.
“When I had the implant removed I went for a consultation at my GP to talk about different contraception but the nurse gave me no information at all really.
“I honestly don’t even know what any other alternatives are that’s why I wanted to talk to the nurse, but she basically just said the pill or get another implant so it wasn’t very helpful.”
And so, Jenni stuck with the implant.
Luckily, it was second time lucky for her as she saw a significant drop in the side effects she was feeling.
“I’m getting on fine with it now, I don’t notice it at all and I haven’t had any new symptoms and the old ones I don’t really notice enough to think ‘oh it’s my implant causing that’ etc.”
Upon reflection, Jenni believes that sexual health clinics are the way forward in terms of all-things contraception.
“The GP just wants to get it over with in my opinion like they are there to diagnose and they don’t even do the implant - they refer to somewhere else that does it.
"That’s why mine was so delayed because the other place was so overbooked I physically couldn’t get an appointment for five months.
“The sexual health clinics are so much more educational and helpful, I think if I had spoken to someone at the clinic for advice on contraception I would have had a better understanding of what was best for me when I was looking to change.”

Jenni knew she wanted a contraceptive she could 'just forget about'.
Jenni knew she wanted a contraceptive she could 'just forget about'.

Jenni is now using the implant for her second time.
Jenni is now using the implant for her second time.

Roxanne: "I knew that the implant or the coil wasn't for me."
Roxanne: "I knew that the implant or the coil wasn't for me."

The Sayana Press injection made Roxanne 'spiral into a different person'.
The Sayana Press injection made Roxanne 'spiral into a different person'.
ROXANNE BEVAN: THE INJECTION
21, STUDENT
Some young women find that they swap and change their method of contraception a number of times to work out which they feel most comfortable with. If you’re willing to go through the day-to-day impact each might have until you find what’s best for you, it may be the most sensible path to take. This was exactly what Roxanne did.
Roxanne began to take the Depo Provera injection as her primary form of contraception when she started university, but this wasn’t her introduction to birth control.
She had previously been on the Microgynon pill, a combined pill, throughout her teen years, as a way of managing periods. This didn’t help as much as she felt that the doctors had told her, and it wasn’t until they suggested the Rigevidon pill she decided to take her first break away from contraception.
“At the time I was offered it, I’d had a few friends that were on it and it wasn’t working out, couple that with the masses of reports and news articles surrounding the nasty side effects, I couldn’t consciously continue with the pill.”
A few years later and Roxanne made the mindful decision to research LARCs: “I did research and I knew the implant or the coil wasn't for me, again I'd heard horror stories and I didn't want to go back on to the pill.”
This was how she discovered the injection. The injection needs to be administered every three months at a GP surgery or sexual health clinic. There’s also a number of variations of the injection, or shot, but Roxanne ended up on Depo Provera.
“I made the choice to try to Depo Provera injection and this proved the most effective for myself.
"I was rid of periods, I personally didn’t notice any side effects, my moods were OK and I didn’t gain weight.”
Roxanne feels it's so important to keep track on how your body reacts to a new contraceptive, and to listen to what your body wants. In her case, Depo was the best option.
"I was rid of periods, I personally didn’t notice any side effects, my moods were OK and I didn’t gain weight.”
But Depo didn't just cause no side effects for Roxanne, it actually made her feel better within herself.
“I felt good in my body and my periods stopped which meant I was no longer anaemic or in pain and that was the thing that was the biggest effect for me.
"I was much happier and able to lead a better life, I'd just moved away to university so I would've noticed any changes to my moods but overall it was a really positive experience for me and even when withdrawing from Depo, I've had tests on bone function etc. and luckily nothing was affected.”
Roxanne chose to continue with the Depo Provera for the next two years. After that time, her contraceptive journey became disrupted.
"I gained weight rapidly and it made me feel alien within myself."
After a period of time, some women who use the Depo shot can be asked to switch to Sayana Press, an alternative, by sexual health teams.
“They then asked me to switch to Sayana Press - an injection that you do at home yourself which I tried and this ultimately ended my journey with contraception because I hit a really bad space with my mental health due to adverse side effects.
"I gained weight rapidly and it made me feel alien within myself."
The Sayana Press injection is one that can be administered from home and is injected into the stomach as opposed to the muscles in the hip and bum area. Those who use it are asked to have one session of it administered in a sexual health clinic to learn how it is injected, and on the second visit they can take home supplies with them. After three months, Roxanne didn’t attend the second session.
"I started to spiral into a different person."
“I never made it to my second session because after two weeks - Sayana Press is known to metabolise quicker than Depo due to the injection site - I’d noticed considerable mood changes. I started to spiral into a different person."
"I was moody, snappy, I didn’t want to go anywhere or do anything, I had little to no interest in my partner, began breaking out really badly with acne but on my back as supposed to my face, I gained around one and a half stone.”
It was at this point Roxanne decided to stop with contraception. After several years of going between the pill then to injections, she felt as though it was only fair to give her body a break.
“I did think about going back into Depo Provera but after putting my body through it for two years and suddenly switching to something else, I knew I needed a rest.
“I definitely think that with active research and knowing your own body, knowing that there are other options there and you don’t have to sit back and take it, there will be a decreased use in the pill.”
KIELE-ANN DUNNE: THE COIL
23, STUDENT
However, unlike Roxanne, some girls don’t choose to shop around but find themselves pushed and pulled between different contraceptive options. Kiele-Ann was left with no choice, a number of times, but to change her form of contraception. Now, she says, she’s discovered the coil and is the best thing that’s happened.
Kiele-Ann made the decision to have the implant as her first form of contraceptive. The choice was made as she could forget it was there. But not all was as well it is first seemed.
The implant is supposed to be replaced every three years, but just a year and a half in, she was having it removed.
“It gave me really bad migraines and pains in my upper arm. It made my periods very irregular and when I did get a period they were awful. I had the worst mood swings so it really didn’t agree with me.”
Now without the implant, Kiele-Ann needed another form of contraceptive. She ‘defaulted’ to the progestogen-only pill, due to her history of migraines. Thinking this change was exactly what her body needed, she was proved wrong.
“The pill sent me spiralling into depression, made me gain weight, my mood swings were worse, and it was all round awful.”
Things seemed to go from bad to worse, which took a significant toll of Kiele-Ann's mental health.
“The pill sent me spiralling into depression, made me gain weight, my mood swings were worse, and it was all round awful.”
Due to the horrific side effects Kiele-Ann had spent 18 months putting up with the implant, it took her a long time to make the link between these new side effects and the pill.
“I didn’t realise it was the pill having these effects at the time. So I was on the pill for a couple years with no check-ups from the doctors, which felt strange.”
After almost three years on the pill, Kiele-Ann decided that all of these harmful side effects were having nothing but a negative impact on her daily life, she discussed the option of stepping away for contraception altogether, and used condoms only.
“My mood started to lift and mood swings were improving.”
The break did Kiele-Ann wonders in terms of feeling more herself.
“My mood started to lift and mood swings were improving.”
The uptake of LARC options are more often than not taken by young women who are in long-term relationships and need something reliable that isn’t just the male condom. After about a year of just using condoms, Kiele-Ann realised she needed to do this too.
She spoke to sexual health teams to enquire about what her options were, to hopefully find something that wouldn’t play havoc with her hormones again.
“The nurses told me after I explained my history that anything with hormones is not ideal for me, so they recommended the copper coil. That was the first time I ever felt listened to.
"It took for me to have to go through an awful ordeal to be listened to and helped genuinely. I agreed to the copper coil and got it fitted this year.”
There’s variations of the coil: namely the copper coil and the mirena coil. The copper coil is not hormonal. Once the coil is fitted it can last between five to 10 years as a 99% effective form of contraception, but some girls turn away from it as it can be deemed invasive.
“It was incredibly painful when they fitted it, and gave me awful cramps and bleeding for a week after the fitting.
"But since then the pain has decreased. My periods are more heavy now and I still get bad cramps for the days of my period and a few random ones.
"However, I have had no other side effects. And the cramps are controllable with paracetamol and ibuprofen. I was told clearly about the pain, so none of this was a surprise for me.”
“I am very happy on the coil, I don't even know it’s there."
Despite the awkwardness of its fitting, after just a few months Kiele-Ann already felt different. This time, and finally, in a good way.
“I am very happy on the coil, I don't even know it's there. My periods are the most regular as they have been since the pill etc., and I'm not miserable or depressed.
"Its the best thing I've done.
"It's a real shame it took for me to have to do one of the worst things imaginable to even be told about it.”

Kiele-Ann was taken off of the implant just half way through its three-year course.
Kiele-Ann was taken off of the implant just half way through its three-year course.

Kiele Ann, coming off of contraception: 'my mood started to lift'.
Kiele Ann, coming off of contraception: 'my mood started to lift'.

Mollie: “I’ve never had children so I was terrified! It sounded horrible.”
Mollie: “I’ve never had children so I was terrified! It sounded horrible.”

Mollie's mental health hasn't been negatively affected by the coil.
Mollie's mental health hasn't been negatively affected by the coil.
MOLLIE MANNING: THE COIL
23, PHOTOGRAPHER
Getting the coil can be quite an invasive procedure, and if not inserted correctly can cause all kinds of uncomfortable problems. This is the main thing that will put many young women off of having it, despite being the longest lasting form of contraception available in the UK.
For Mollie, this was the biggest decision she was having to make in terms of her health, and so took the time to consider it.
Mollie started her contraceptive journey on the Microgynon pill, a version of the combined pill. One of the most significant side effects she felt from it was nausea, which affected almost every element of her life.
“I was a waitress at the time so I kept on having to cancel work due to being sick - you have to have 48 hours off because you’re dealing with food - so yeah, my managers loved me!”
Mollie sought out an alternative, the next pill she tried was no better, nor was the different one which followed, or the mini-pill which came after.
“For the whole week on my periods I’d have horrific headaches, once I had a migraine, I was throwing up and had diarrhoea it was horrible!"
Four different pills later and Mollie was still feeling nauseous nearly all of the time.
“For the whole week on my periods I’d have horrific headaches, once I had a migraine, I was throwing up and had diarrhoea it was horrible!
"And then the other times of the month I would just be feeling nauseous and have headaches.
"None of it worked until I came off of it and tried something else.
“To help me not be sick, doctors suggested an option for something that didn’t have to go through my digestive system.”
She was offered the coil, but having heard about how invasive it could be, the procedure alone was a daunting thought.
“Due to me being under 25 I’ve never had a smear test and I’ve never had children so I was terrified! It sounded horrible.”
With getting the coil, women must have a coil consultation to discuss everything, even before the procedure is done. Mollie expressed how she felt, and was offered the contraceptive patch for the time being.
“So I had a coil consultation anyway and in that consultation I was offered to try the patch. Which I did and it worked for over two years!
"I really got on with it apart from it sometimes falling off on holiday with being in the pool and in the sea. But that seemed like a small price to pay.
“I then started to get really itchy, spotty and rashy around the area the patch would be in so then they told me I had started to become allergic to it.”
Having time between the first and second coil consultation, Mollie realised a longer lasting form of contraception was definitely the way forward for her. She says that it was this time that solidified her wanting to take up this commitment.
“The patch bought me some time so I was able to process what needed to happen next, so when the time came - because the patch for me was only ever temporary - that when they said ‘OK you’re allergic’, I said I was ready to have another coil consultation and have it put in.”
Mollie believes it has been the best option for her so far and is currently enjoying it.
"My symptoms since the coil have calmed down a lot."
The only side effect Mollie has noticed is that her skin has broken out.
“My symptoms since the coil have calmed down a lot.”
“I think it’s much more of an ‘accepted’ form now. As they can make them small so you don’t need to have had children to have one put in, so more young women are having them.”
